Teethforhealth.com
- About Us
- Disease Risk Assessment
- …
- About Us
- Disease Risk Assessment



Teethforhealth.com
- About Us
- Disease Risk Assessment
- …
- About Us
- Disease Risk Assessment

Tooth Decay
Tooth Decay (dental caries), is a loss of tooth structure caused by bacteria breaking down sugars and the subsequent release of acids. If tooth decay is left untreated, it can cause severe pain and swelling, resulting in tooth loss.

Tooth Decay happens as a result of several factors, including bacteria (plaque), sugar intake frequency and time*.
Bacteria - microorganisms that can digest sugars from your diet
Sugar - source of energy that bacteria needs to grow and cause decay
Time - tooth decay is a long-term process and doesn't happen overnight
*If you remove one or more of these factors, tooth decay may be preventable and even stop progressing entirely.

There are many patterns of tooth decay, and the exact size/depth can be unpredictable.
Gum Diseases
Gum diseases can be roughly classified into 2 categories:
1. Gingivitis - a reversible form of gum disease caused by dental plaque, usually appears as bleeding when brushing and redness of gums
2. Periodontitis* - an irreversible, advanced form of gum disease that involves pocket formation, gum recession and bone loss, resulting in mobility and subsequent loss of teeth

Risk factors including genetics, poor oral hygiene, smoking and poorly controlled diabetes can increase the risk of development/severity of gum diseases/treatment outcome.
*Requires ongoing reviews and further management by dental practitioners

A periodontal chart is required to understand the extent and severity before intervention.

Advanced gum disease with heavy calculus/tartar deposits and gum recession: gums appear red and swollen.
Oral Cancer
Oral Cancer can appear as various forms:
- A painless ulcer that doesn't heal >3 weeks,
- A slow growing granular swelling,
- Rough crusts/eroded area on the lips, &
- White/red patches in your mouth.


Risk factors of oral cancer include smoking, excessive exposure to sunlight, excessive alcohol consumption, chewing of tobacco and paan (betel leaf with Areca nut), HIV etc.
Do not put yourself into unnecessary risk! Contact your dental practitioner and get a dental check-up regularly for cancer screening.
*Oral cancer assessment requires specific clinical procedures such as a biopsy, and cannot be confirmed by just visual screening.
Bad Breath
Bad breath is also called as halitosis. Most people are not aware their mouth produce a 'rotten egg' smell. Up to 90% of bad breath cases come from the mouth.
Type of bad breath:
- Transitory; caused by food e.g. onions and usually last for 24-72 hours
- Chronic; associated with a certain dental condition e.g. decay, gum disease, poor tongue hygiene, broken fillings etc.
- Medical; associated with a certain medical condition
Depending on the type of bad breath, the treatment will vary in time and difficulty. Using breath fresheners and mouthwashes may help a bit temporaily, but not resolving the problem completely. Occasionally, it may be caused by a medical condition.
What can I do?
- Book a thorough dental examination to confirm potential dental causes
- Maintain a good oral hygiene including tongue cleaning
- Maintain regular dental cleaning
- Use of special mouthwashes as recommended by your dental practitioner
- Visit a medical practitioner if needed*
*Requires ongoing reviews and a dental referral may be required
Sensitive Teeth
Sensitive teeth can impact your eating experience. It is important to determine its exact nature and receive treatment as soon as possible.

Gum recession
Gum recession is mainly caused by periodontal disease, aggressive brushing and/or use of abrasive products. When gums recede, roots will be exposed and they can be very sensitive to temperature and pressure. Continuous hard brushing can exaggerate the sensitivity and makes it harder to be managed conservatively.

Tooth decay
Tooth decay exposes inner structure (dentine). When bacteria gets closer to the nerve tissues, hot/cold things can be directly conducted and amplify the sensations, thus causing sensitive teeth.

Grinding/clenching (bruxism)
Grinding your teeth can wear them down and even cause the teeth to flex along the gum line (abfraction). Continuous grinding habit can cause many dental complications on the long term.

Dental erosion/erosive wear
Dental erosion is usually caused by an acidic diet (alcohol, soft drinks and citrus) and gastroesophageal reflux disease (GERD). Since the acid will corrode the teeth, inner structure (dentine) will be exposed and cause dentinal hypersensitivity. Placing fillings on erosive wear can be difficult and they tend to last shorter.
Brushing Abrasion
When you brush with the wrong technqiue, an unsuitable toothbrush and use abrasive oral products, brushing abrasion/abrasive wear can happena and progress irreversibly.
Most common treatment options:
- Cause(s) and relevant risk factors must be identified
- Progression must be monitored regularly
- Using a soft toothbrush with the correct technique, pressure and duration
- Avoid using abrasive products e.g. whitening toothpastes
- Sensitive toothpaste to relieve symptoms
- Restorative treatment if needed

Consequences 1: Gum recession, exposed roots and tooth sensitivity
Gum recession can happen with abrasive wear. When gums recede, roots of the teeth are exposed and they can be very sensitive to temperature and pressure. Continuous hard brushing can exaggerate the sensitivity and makes it harder to be managed conservatively.

Consequences 2: Tooth decay and crown fracture
When more roots wear away with ongoing hard brushing, notches on roots along the gum line become deeper and bigger. Brushing can become difficult and the risk of tooth decay increases. Besides, the strength of the tooth along the notches becomes weaker, and abfraction can happen. The crown can potentially break and tooth removal may be required.

Consequences 3: Aesthetics
With exposed roots and the present of abrasive wear, your appearance can be compromised because of their shapes and a more yellowish colour. They can be challenging to manage with conservative treatment and other restorative options can be expensive and difficult.
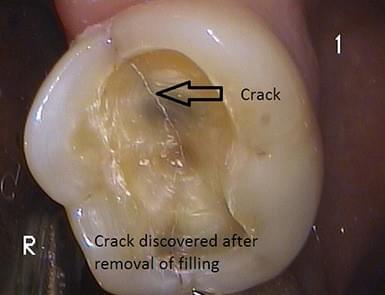
Cracked Tooth
A cracked tooth can have signs and symptoms of:
- Pain on biting and/or when releasing your bite
- Sensitivity to hot and cold, or sweet things
- Persistent pain cycle

Causes:
Grinding/clenching habits
Grinding/clenching habits and chewing on hard things can add extra pressure on teeth, and make them more vulnerable to fracture.
Large fillings (especially old metal fillings)
Teeth are mechanically weaker after fillings. The large the filling, the weaker the tooth,. A crack can extend as time goes and cause symptoms eventually, especially when the filling isn't checked periodically, isn't in a good condition (marginal leakage) and not well maintained.
Treatment options will be determined by the degree of the crack and severity of symptoms. If the crack is detected earlier, more treatment options can be discussed and the chance of saving the tooth is generally higher. However, if the crack is too large and deep, the tooth may need to be removed.
Bruxism
Teeth grinding/clenching is a physical wear caused by tooth-to-tooth contact. It can cause damage to your teeth, alveolar bones and jaw joint.

Causes and signs:
It can happen subconsciously during day and night time. There is a higher risk when you are concentrated on doing something or stressed about something.
- Friction rub sound
- Teeth wear - flattened or chipped surfaces, abfraction
- Teeth sensitivity - exposure of yellowish, deeper layers (dentine)
- Unwanted teeth movement
- Clicking of jaw joint, even a locked jaw
- Pain/soreness of jaw joint and jaw muscles
- Increased attachment loss of existing periodontal diseases
- A higher risk of broken fillings

Treatment options (short and long term):
- MOST IMPORTANT: explore the actual cause(s)
- Jaw exercising
- Soft diet
- Heat packs and massages (only for jaw muscle soreness and pain)
- Occlusal splint therapy (nightguard)*
- Botox injection (for locked jaw and mild jaw muscles)
- Surgery
- Myotherapy
- Treatment by a dental/medical specialist if symptoms cannot be relieved
Additional treatment
- Simple/complex orthodontics/restorative procedures as deemed necessary
- Medication(s) from a medical practitioner as deemed necessary
- Referral to another health practitioner(s) e.g. psychologist, physiotherapist, surgeon etc.
*An occlusal splint is a plastic custom-fitted oral appliance for your to wear at night, which provides a cushioning effect for both upper and lower teeth and minimizes the extent of jaw movement.
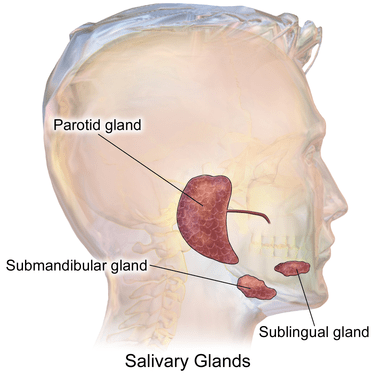
Dry Mouth
Dry mouth (xerostomia) refers to a condition that the salivary glands in your mouth don't make enough saliva to keep your mouth wet. It can become a major problem since saliva helps to prevent tooth decay, enhance your ability to taste and chew, and aid swallowing and digestion.
Common symptoms of dry mouth:
- Dryness/stickiness in your mouth
- Thick and Stringy saliva
- Bad breath
- Difficulty chewing, speaking and swallowing
- Dry/sore throat
- Dry/grooved tongue
- Change in sense of taste
- Problems wearing dentures*

Causes:
Medications
Certain medications, especially for diabetes and depression, produce dry mouth as a side effect.
Aging
Elder people experience dry mouth due to the use of certain medications, the body's ability to process medications and inadequate nutrition.
Cancer therapy
Both radiation therapy and chemotherapy drugs can change the nature, the amount of saliva and structure of salivary glands. The effect may be temporary or permanent, depending on the dose and area treated.
Use of tobacco and alcohol/alcohol-containing products
Both tobacco and alcohol can exaggerate existing dry mouth.
Recreational drug use
Drugs including methamphetamine and marijuana can cause dry mouth and "meth mouth".
Medical/dental conditions
Medical conditions such as yeast infection, Alzheimer's disease, HIV/AIDS and Sjogren's Syndrome can cause dry mouth. Dental conditions such as salivary gland blockage and extensive surgical procedures can cause temporary/permanent damage.
Snoring/mouth breather
Snoring or breathing with your mouth open can exaggerate dry mouth.
Treatment options will be determined by the cause(s) and severity of symptoms. Most options are cause dependent.
*You should always consult a dental practitioner to consider other underlying issues with the dentures.
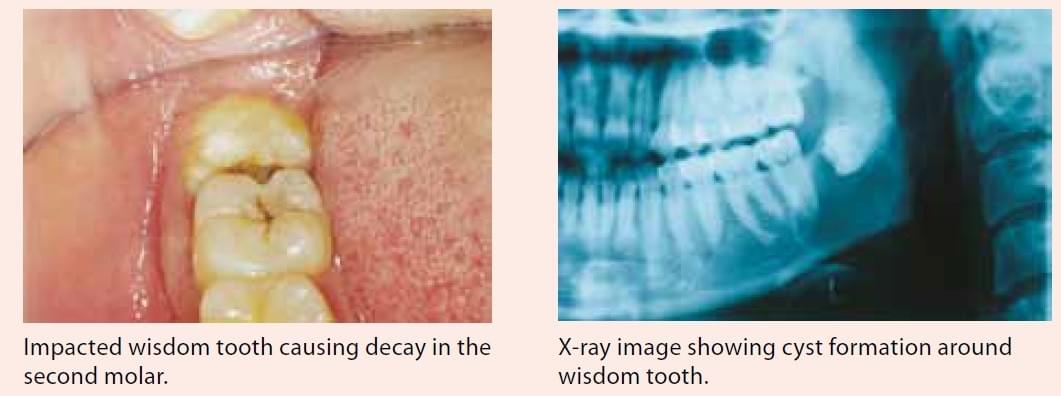
Impacted Wisdom Tooth
Impacted wisdom tooth can be a tricky dental problem since it doesn't always cause symptoms while doing severe damage to other teeth. The problem usually happens between the ages of 17 and 25.
Common symptoms of impacted wisdom tooth:
- Swollen gums at the back
- Tender or bleeding gums
- Jaw pain overnight
- Swelling around the jaw
- Muscle tenderness
- Bad breath
- An unpleasant taste in your mouth
- Difficulty opening your mouth
- Facial swelling, fever, sore throat and difficulty breathing (in severe cases with infection)

Problems you may get from an impacted wisdom tooth:
- Damage to other teeth e.g. root resorption
- Tooth decay
- Gum diseases and bone loss
- Cyst/tumour (mostly benign)
- Crowding of other teeth

How do I prevent impaction of wisdom tooth?
Unfortunately, it is not possible to control the position/angulation of how a wisdom tooth grows. Therefore, removal of wisdom teeth may be inevitable. One of the purposes of having regular dental visits and x-rays is to monitor the growth and emergence of wisdom teeth, evaluate the risk and detect problems earlier.
Golden rule: cost to repair damages caused with wisdom tooth impaction is higher than cost to remove impacted wisdom tooth
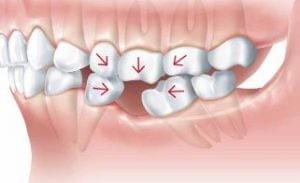
Missing Tooth
There is always a chance when you lose a tooth due to oral diseases including tooth decay, gum diseases or cracked tooth. Some people do not have all permanent teeth. A missing tooth can cause severe complications to one's chewing, smiling and the health of other teeth.
What can you do*?
*Please consult your dental practitioner to discuss available options. Options are dependant on each individual's oral environment.

Option 1 - Do nothing
Pros:
- No cost involved
Cons:
- Teeth drifting
- Over-eruption
- Imbalanced load distribution
- Food impaction
- Compromised bone support

Option 2 - Partial denture
Pros:
- Improve aesthetics and/or chewing
- Comparatively affordable
- Suitable for multiple missing teeth
- Relatively low cost
Cons:
- Shortest life span
- Good denture hygiene required
- Regular adjustments required
- Can be uncomfortable (removable)
- Metal components may be visible (depends on design)
- Cannot prevent shrinkage of gums and bone

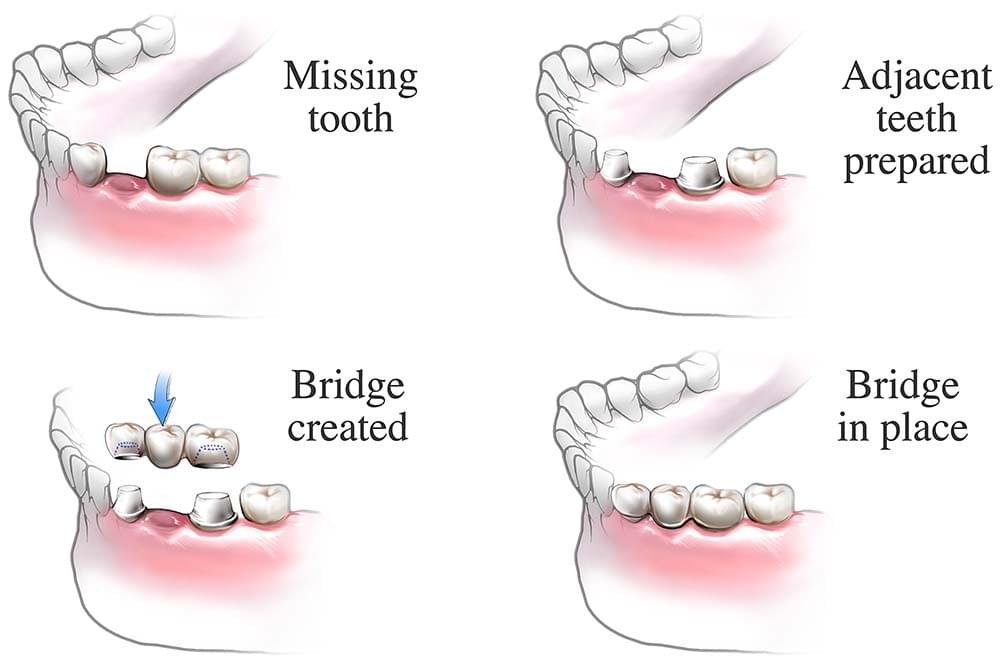
Option 3 - Dental bridge
Pros:
- Good stability (fixed)
- Good for single tooth replacement if adjacent teeth are heavily filled
- Long life span (~10+ years)
Cons:
- Relatively higher cost
- Good bridge hygiene required
- Higher requirement on adjacent teeth e.g. stability, health
- Need ongoing reviews and professional care

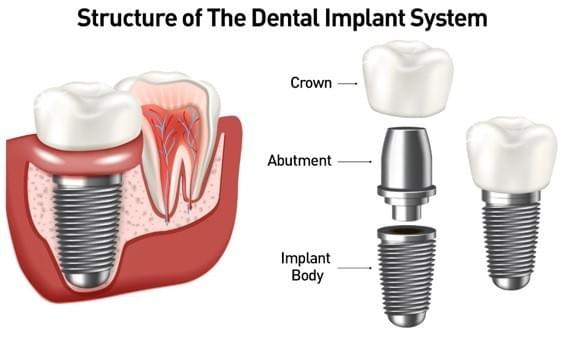
Option 4 - Dental implant
Pros:
- Good stability (fixed)
- Good aesthetics and functionality
- Feel very similar to a real tooth
- Long life span (~20+ years)
- Can be used to replace multiple missing teeth
Cons:
- Relatively high cost
- Surgery required
- Good implant hygiene required
- Higher requirement on the health of the overall oral environment
- Need ongoing reviews and professional care
- Must avoid certain habits e.g. smoking and chewing on hard things
Malocclusion
Malocclusion is referred as a list of poor arrangement of teeth. They can impact your chewing ability, appearance and health of your teeth and supporting structures around. Your upper jaw teeth should slightly overlap with your lower jaw teeth so that the pointed ridges of your upper molars fit into the grooves of your opposite molars.
Orthodontics can solve the issue, whether it is an underlying dental issue, jaw problem or a combination of both! Most treatment plans involve multiple procedures as listed below:
- Braces to correct the position of your teeth
- Dental appliances or aligners to change jaw position during growth or realign teeth
- Removal of teeth to correct overcrowding
- Reshaping, bonding, or capping of teeth
- Surgery/surgical treatment to reshape or shorten your jaw